Mucosal Damage
Reviewed by: HU Medical Review Board | Last reviewed: June 2024 | Last updated: June 2024
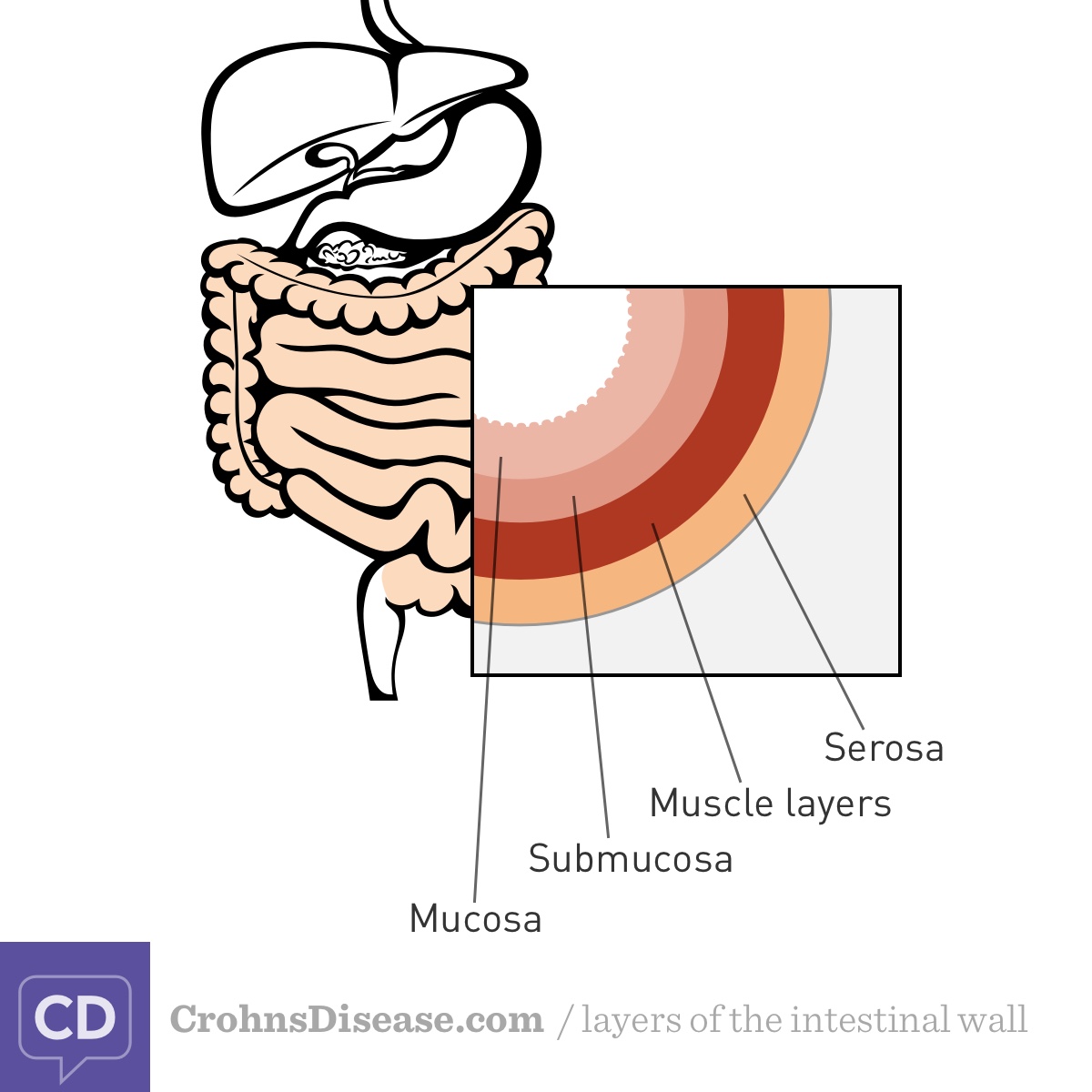
Inflammatory bowel disease (IBD) causes ongoing (chronic) inflammation. This damages the walls of your intestine. Crohn’s disease and ulcerative colitis (UC) are the 2 main types of IBD. Crohn’s disease can affect any layer of the intestinal wall. UC typically affects only the inner lining of the wall. This lining is called the mucosa.1,2
Mucosa is another word for mucous membrane. These are areas of soft tissue that line your organs and the entrances to your body. Your mucosas protect you from harmful substances. Your entire digestive tract, from your mouth to your anus, is lined with protective mucosa. IBD harms this mucosa.2,3
Figure. Layers of the intestinal wall
Why does IBD cause mucosal damage?
The mucosa in your digestive tract does several important jobs, including:2,3
- Helping to protect your stomach from being damaged by the stomach acids that break down your food
- Keeping harmful organisms from passing from the gut into the body
- Releasing digestive enzymes that help you absorb nutrients from your food
Experts think that in people with IBD, the immune system mistakenly attacks the cells in the intestinal wall. This causes chronic inflammation that damages the mucosa. Over time, the mucosa breaks down in certain spots. Wounds called ulcers or lesions result. These damaged areas can allow harmful bacteria and other substances to pass into the body.4
In people with UC, inflammation and ulcers occur in the large intestine (colon or rectum). People with Crohn’s can develop ulcers anywhere along the digestive tract. But their damage most commonly occurs in the small intestine and the first part of the large intestine.1
How does mucosal damage affect people with IBD?
There is much that experts do not fully understand about IBD. For example, researchers are still exploring the link between mucosal damage and IBD symptoms. But damage to the mucosa may lead to many common IBD symptoms, including:4
- Diarrhea
- Abdominal pain
- Rectal bleeding
- Malnutrition
In severe cases of IBD, especially Crohn’s disease, mucosal damage also may lead to complications such as:1
- Scarring (fibrosis)
- Places where the intestinal wall is so narrow that it is hard for food to pass through (strictures)
- New, abnormal connections between the intestine and other organs (fistulas)
- Holes in the intestinal wall (micro-perforations)
Extreme cases of IBD can lead to a life-threatening condition called toxic megacolon. This happens when prolonged inflammation spreads to the muscle layer of the colon wall. The muscles in the colon wall freeze and stop moving contents through the colon. These contents then build up, releasing toxins. The colon muscles also widen and stretch. This lets the toxins leak into the rest of the body.5
How is mucosal damage diagnosed?
Doctors usually use endoscopy to diagnose IBD. This procedure involves inserting a long, thin tube (or capsule that you swallow) with a tiny camera and light into the digestive tract. The camera lets your doctor see areas of mucosal damage or inflammation. Common types of endoscopy include:6
- Colonoscopy to look at the rectum, colon, and last part of the small intestine
- Flexible sigmoidoscopy to look at the lower colon and rectum
- Upper endoscopy to look at the esophagus, stomach, and first part of the small intestine
- Capsule endoscopy to look at various parts of the digestive tract
During an endoscopy, your doctor may take a small tissue sample to look at under a microscope. This is called a biopsy. Your doctor may also gather information using:6
- Blood tests
- Stool tests
- Other imaging tests
How is mucosal damage treated?
Many IBD treatments focus on reducing inflammation and the long-term damage it can cause. Reducing inflammation may reduce symptoms and complications. It also can give any existing damage to your mucosa time to heal. Some treatments focus directly on healing the mucosa.4,6-9
Researchers are actively studying new medicines to help with mucosal healing. For now, drugs commonly used to treat IBD include:6-9
- Aminosalicylates, such as sulfasalazine, mesalamine, olsalazine, and balsalazide
- Corticosteroids, such as prednisone and methylprednisolone
- Drugs that suppress the immune system, such as azathioprine, mercaptopurine, upadacitinib, and ozanimod
- Biologics and biosimilars, such as infliximab, adalimumab, golimumab, and natalizumab