What Is Pelvic Floor Rehabilitation?
People whose inflammatory bowel disease (IBD) is in remission can still experience gastrointestinal (GI) symptoms. These symptoms may include an inability to control their bowels, known as fecal incontinence. Constipation is also a common problem.1
Dealing with bowel symptoms can lead to depression and anxiety. It may also make people less productive at work or at home. People with IBD often change their lifestyles to avoid situations where their symptoms might embarrass them. But this avoidance limits their working, social, and personal lives.1
Feelings of shame and embarrassment may prevent you from telling your doctor about all your symptoms. And your doctor may not see that there is a problem if tests show that your IBD is stable. But if you are having symptoms, especially when you are considered to be in remission, a behavioral treatment called pelvic floor rehabilitation may help.1
Behavioral treatment for Crohn's and ulcerative colitis
Behavioral treatment programs for Crohn's disease or ulcerative colitis address both physical and mental factors. Exercise and diet changes are often included in these programs. Bowel habit training also may be included. This is because it is common for people with IBD to have overactive muscle activity in response to their IBD symptoms.1,2
Bowel habit training is led by a physical therapist. The training encourages going to the bathroom at a predictable time, including right after meals. Frequent bathroom visits are discouraged. So is straining to have a bowel movement. Bowel habit training can go hand in hand with pelvic floor rehabilitation.1
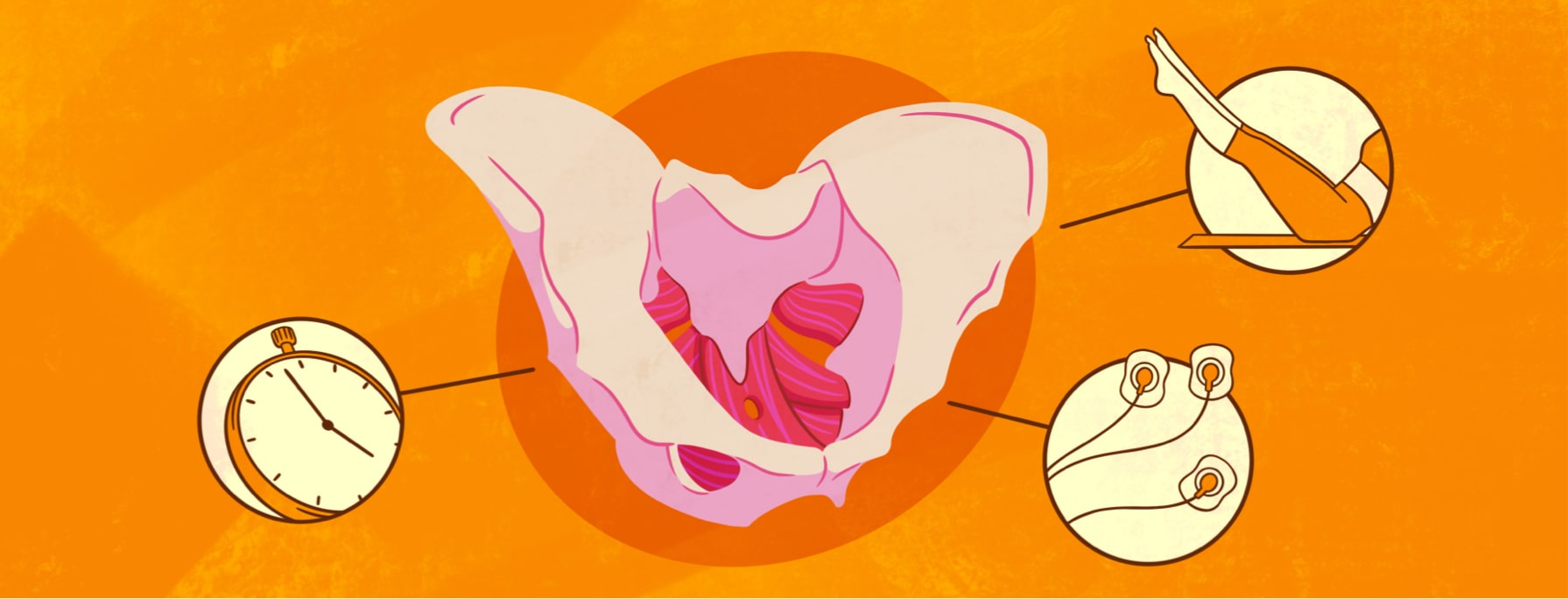
Learning about the pelvic floor
It is helpful to know a bit about the GI system and the muscles that help it work. These muscles include the:1
- Diaphragm
- Abdominal wall
- Pelvic floor
The muscles of the pelvic floor hold your pelvis, bowel, and bladder in place. These muscles also support your reproductive organs. And they help you control your bladder and bowel function, which is known as continence.3
Pelvic floor exercises and rehabilitation
Problems with the pelvic floor muscles are addressed through pelvic floor rehabilitation. The goal of pelvic floor rehabilitation is to improve the strength, endurance, relaxation, and coordination of the pelvic floor.1,4
Pelvic floor rehabilitation also targets the abdominal muscles, the diaphragm, and the anal sphincter to help with IBD symptoms. The anal sphincter is a ring-shaped muscle at the opening of the anus. This muscle relaxes or tightens to open or close the anus.1,4
Kegel exercises, or Kegels, are a key part of this treatment. To perform Kegels, squeeze the muscles you would use to prevent passing gas. You should feel a pulling in your vagina or rectum. Hold the squeeze for 3 seconds, then release the muscles and relax your pelvic floor. The goal is 10 to 15 repetitions every time you do Kegels.1,5-7
Other types of pelvic floor training
Pelvic floor training can include a wide range of treatments. These treatments may include:3,5,8
- Exercises that focus on your core strength and posture, including Pilates
- Inserting thin needles into trigger points to increase blood flow, decrease muscle tightness, and reduce pain
- Electromyography (EMG) biofeedback, which uses sensors to get information about your pelvic muscle activity. This information helps therapists design exercises to retrain and strengthen your pelvic floor muscles.
- Myofascial release, a type of massage that targets the membranes that support and connect your muscles. Massaging these trigger points in the pelvic floor reduces pain.
- Using mild electrical current to stimulate a muscle. The goal is to strengthen the muscle and normalize nerve activity.
- Laser therapy to heal muscles on a cellular level.
Does it work for people with Crohn's or UC?
A 2022 study found that behavioral treatment led to less severe IBD symptoms. Almost three-quarters of people in the study reported moderate or significant improvement in their symptoms. A 2019 study had found similar results. In that study, 77 percent of people reported that their fecal incontinence was much better after treatment.1,9
While it may be uncomfortable to speak with your doctor about your IBD symptoms, it is important. A physical therapist can help you create a pelvic floor rehabilitation plan that can make your day-to-day life less stressful and more fulfilling.
Join the conversation