It's Back: Another Painful UC Flare
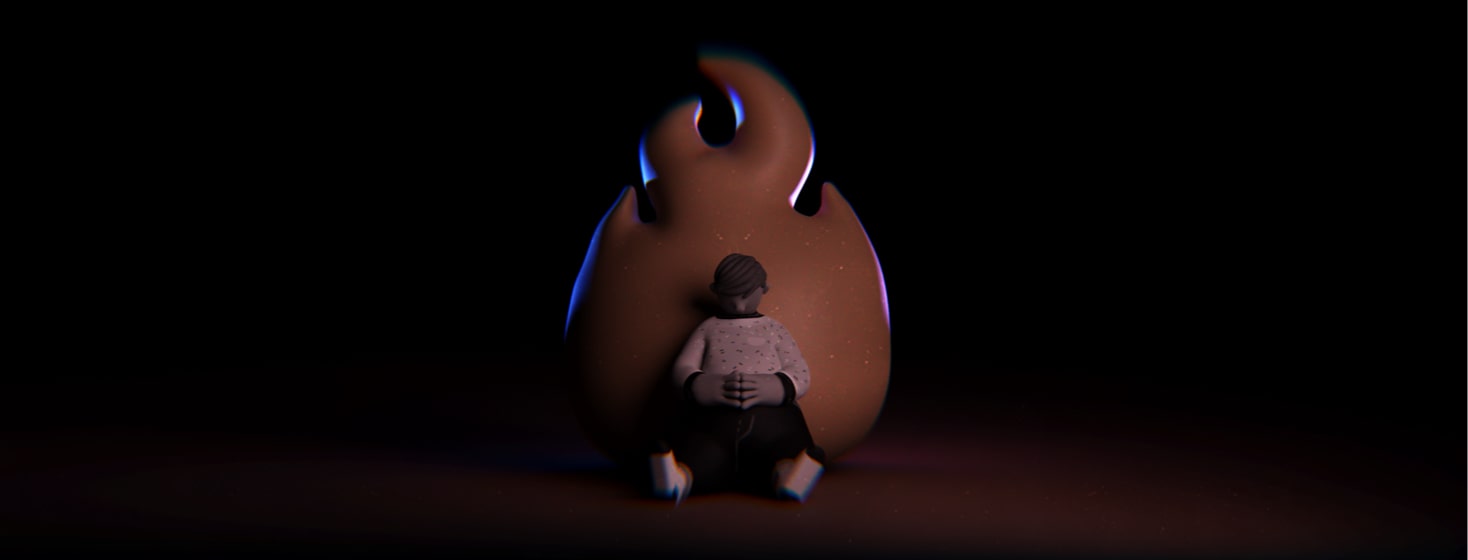
The pain is back. Like a jackhammer in my gut, I feel the pulsating, rippling high-tide of pain throbbing throughout my belly. As I draft these words, I sit hunched over my keyboard as a colitis flare has signaled its return.
Last year, I wrote an article about my shadowy companion called "Flare." Those with IBD understand that we are never free of Crohn's or UC flares. After 30 years, I thought I had figured out my colitis. But then life happens and before I realized it, a flare slowly crept to the surface.
I try to avoid my flare triggers
First, let me explain that I consciously apply techniques to avoid triggering flares. I watch what I eat, take specific multivitamins, exercise, and meditate daily. For my body, I've just learned to stick to a routine to avoid disrupting my digestive system. Most often, this regiment works.
But the past couple of years have brought an unwelcome guest into my life. Its name is "Stress," and I'm not a fan of it. At this moment, my body is telling me I need to take proactive steps against this visitor.
You see, I'm a public high school teacher. As such, I've been dealing with behaviors and issues that I've not experienced during all my 30 years in the classroom. Since 2020, the increase in mental health issues and behavioral problems has grown exponentially in teenagers, and my body has signaled this year that I'm stuffing down all of this heavy load internally. What I stuff inside eventually rises to the surface, bubbles, and spills out the only way it knows how – through a flare-up.
When UC flare symptoms start showing...
At first, it started quietly. Looking back, I would say it began quite subtly. I noticed mucus in my stool. But I figured I would watch my food intake better, incorporate more breathing exercises, and increase my typical exercise routine a bit more.
Then, the blood arrived with my bowel movements. At that point, I thought, "Hmm... Am I starting a flare?" But I didn't want to empower this notion. I thought, "If I don't focus on it, my body might just correct itself."
When the sinus infection arrived next, my NP prescribed an antibiotic, and I got distracted by a clogged nose and an incessant cough. Little did I even think about the antibiotic because I was just focused on the gunky congestion.
But once bloody diarrhea and gut pain arrived, I knew for sure I was experiencing a UC setback.
Pain, diarrhea, exhaustion
So, here I sit, slumped over in pain with my shadowy companion... once again. A flare communicates that I need to get control of my stress levels and wean myself off the antibiotic. The double punch from these 2 sources just hits too hard.
Although I could drone on about the stress of being in the classroom and about the symptoms of my current flare, I choose instead to focus on getting back on track. It does me no good to fixate on the negativity.
So, the first step I take is to grab some Imodium AD. This over-the-counter product is the only way I can continue teaching from 8:00 a.m.-3:00 p.m. each day. It's not good if diarrhea has me running to the restroom. Stopping the diarrhea stands as the most important priority.
Treating painful UC flares
Next, I will search my medicine cabinet. In my bathroom, I found I still have some mesalamine suppositories. I'll start taking one before bedtime. Experience has taught me that I can only handle it for about 2 weeks before headaches begin as a side effect. I'm hopeful my flare will be gone at that time.
Probiotics
Also, my NP has prescribed me a probiotic while I'm on the current antibiotic for the sinus infection. It should help reduce diarrhea while I'm finishing the antibiotic. I'm hopeful that acidophilus will promote good gut bacteria as the antibiotic depletes it.
I've learned that I should take the probiotic either 2 hours before or 2 hours after I take the antibiotic. Apparently, they're not effective when taken together. (Let this flare serve as my reminder.)
De-stressing
Now that I've attacked my flare through the medicinal route, I plan to find ways to relax. So, each night, I'll return to soaking in Epsom salt before heading to bed. It's been a while since I soaked in the tub, but I've always found Epsom salt to be soothing. Plus, I'll add soft, meditative music while doing some reading as I soak the stress away.
How long do my flares last?
So, what's my timeline? Personally, I'm giving myself 2 weeks to turn this flare around. If I can't, then my next course of action will be to contact my GI and request a stronger approach. Is this the best approach for everyone? No.
Above all, I’ve learned in this community forum that UC looks different in everyone. No 2 bodies react the same to the shadowy companion called "Flare." We all need therapies that work best for our own bodies. That path is always done through trial-and-error. I've learned that I try to give my body time to adjust.
Managing a painful UC flare
Maybe I can't control the stress all around me in a classroom. But I can control how I respond to it. For now, I have 2 more months until summer break. At that point, my body will have time to relax. Then I'll see where the universe leads me. For now, I'm just not going to worry about it. Worrying only hurts me more. So, get behind me stress, I have work to do.
Do you have ideas or ways to get your body back on track when experiencing a flare? Please share your ideas with us. We're all in this together, and your idea just might help someone else.
*Update since I wrote this this article: I contacted my GI, and he has prescribed me a short stint on prednisone. It's not my favorite path, but it will help my body turn the corner. Hopefully, I can make it through the rest of this school year without any other medication. Fingers crossed. Please send out positive vibes. My gut needs it!
Join the conversation