Ulcerative Colitis and Skin Conditions
Ulcerative colitis (UC) is a form of inflammatory bowel disease (IBD) that affects the gastrointestinal tract. It is caused by the body's immune system fighting healthy cells by mistake. Though it is a gastrointestinal disease, UC also may be linked to conditions that affect other areas of the body.1,2
For example, skin disorders are common in people living with UC. According to the Crohn's and Colitis Foundation, up to 20 percent of people with IBD experience skin problems. Various skin disorders can occur with UC. Experts believe these skin disorders may be connected to UC in different ways.1-3
Some skin disorders may be caused by the same abnormal immune function that occurs in UC. There also may be environmental triggers that make people more likely to develop both UC and some skin disorders. Finally, there may be similar genes involved in both UC and some skin disorders.1-3
Erythema nodosum
Erythema nodosum (EN) is the most common skin disorder linked to UC. But it does not occur just with UC. It can also be associated with other autoimmune diseases, infections, or medications.2,4
EN appears as tender, red bumps over the shins, ankles, or arms. These bumps are more common in women than in men. They often appear before a flare and will improve as the flare improves.2,4
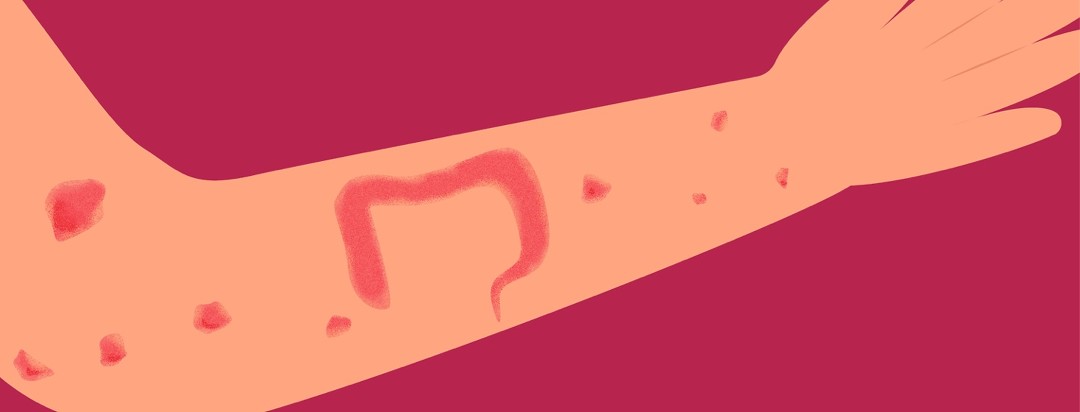
Pyoderma gangrenosum
Pyoderma gangrenosum (PG) is a severe skin condition linked to UC. It most often occurs on the shins or ankles, but it also can appear on the arms.2-4
PG starts as a collection of small blisters. The blisters then join and become a deep, painful ulcer. These ulcers can be caused by a minor injury to the area, like a needle stick or scratch. They may take a while to heal. You may also develop fever, muscle pains, and fatigue.2-4
Psoriasis
Psoriasis is a skin condition that appears as light pink patches on the arms, legs, and trunk. The patches may be covered in dry, silver-gray skin.1
Psoriasis can occur on its own but also is likely to affect those living with UC. Scientists believe that some of the genetic changes (mutations) involved in UC may also be involved in psoriasis. They have also found that the immune processes seen in UC also happen in psoriasis.1
Rosacea
Rosacea is a chronic inflammatory disorder of the skin on your face. It causes facial flushing, skin redness, and bumps under the skin. People with UC are more likely to develop rosacea.5
Researchers have found that the changes to the immune system that happen with rosacea also happen with UC. Both diseases may also be caused by DNA or gene changes.5
Atopic dermatitis
Atopic dermatitis, also known as eczema, is another chronic inflammatory skin condition. It causes red, dry itchy areas that can occur anywhere on the body.1
The inflammation that comes with eczema is caused by the immune system acting abnormally. This disrupts the skin's ability to protect the body from microorganisms like bacteria and fungi. Experts believe that UC and eczema may be caused by similar immune system changes.1,6
Aphthous stomatitis
Also known as "canker sores," aphthous stomatitis refers to ulcers that can occur in the mouth. Anyone can get canker sores. However, they commonly appear during UC flares and may be more severe in those with UC. Severe canker sores can be treated with steroids or medicated mouthwashes.3,4
Rashes caused by nutritional deficiencies
UC causes intestinal inflammation and diarrhea. Because of this, people with UC may not absorb all the vitamins and minerals they need. Important nutrients also can be lost in bowel movements. Low levels of vitamins like niacin, zinc, and vitamins B, C, or K can cause a variety of skin rashes.3
These are not all the skin conditions that can occur with UC. If you have skin symptoms that concern you, talk to your doctor.
Join the conversation