Gallstones
Reviewed by: HU Medical Review Board | Last Reviewed: January 2016. | Last updated: December 2020
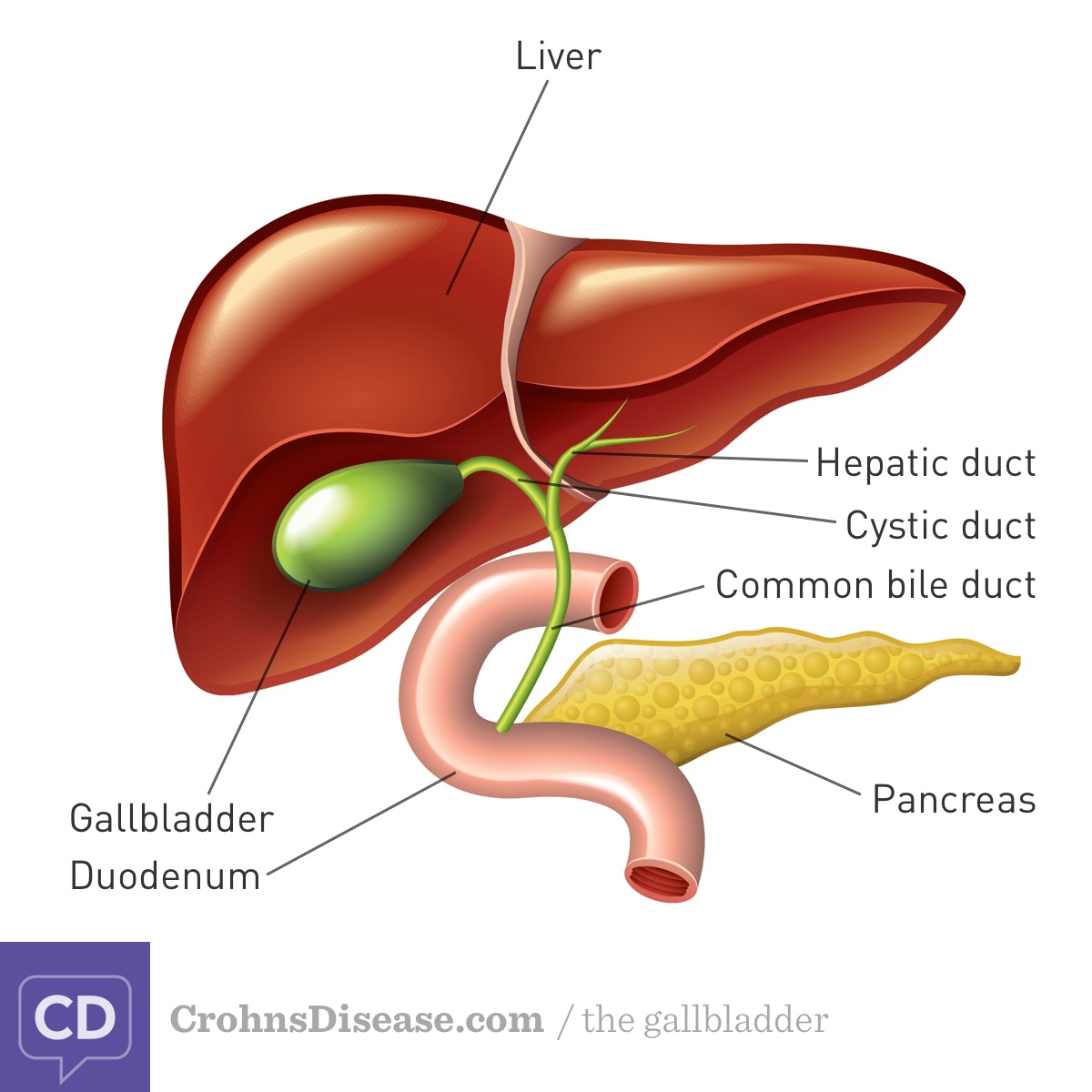
Bile is a fluid that helps you to digest fat.1 The liver produces bile, which is stored in the gallbladder. Bile is made up of water, bile salts, cholesterol, and a pigment called bilirubin, among other things. The gallbladder releases bile into the beginning of the small intestine (duodenum; Figure). The bile salts break big fat drops into smaller droplets. Smaller droplets are easier to for your body break down and absorb. Nearly all of the bile salts are reabsorbed at the end of the small intestine (ileum). They are reused to make more bile.1
Figure. Gallbladder and Bile Ducts
Gallstones are hard particles that form in the gallbladder.2 Another word for gallstones is cholelithiasis. Gallstones are a common problem in the general population and especially in people with inflammatory bowel disease.3,4 One study that compared people with Crohn's disease and ulcerative colitis to the general population found that a person with Crohn's disease had twice the risk of developing gallstones compared to people without inflammatory bowel disease. People with ulcerative colitis did not have an increased risk; however, people with ulcerative colitis can also develop gallstones.5
Overall, about 13% to 34% of people with Crohn’s disease have gallstones.6 Your risk of developing gallstones is particularly high if Crohn’s disease affects your ileum.4
Why is inflammatory bowel disease linked with gallstones?
There are several reasons that people with Crohn's disease are at risk for gallstones:
- Bile salts are not reabsorbed in your ileum. This can happen if the ileum has been removed surgically or it is very inflamed. Instead, the bile salts pass into your colon. Bile salts mix with bilirubin in the colon, changing the bilirubin into a form that can be reabsorbed. Once the bilirubin is reabsorbed, it travels back to the liver to be added into bile. Because there is extra bilirubin in the bile, gallstones start to form. The extra bilirubin makes these gallstones black.4
- If the bile salts are not reabsorbed in the ileum, they pass out of the body. The loss of bile salts means that the liver has fewer bile salts to put into new bile. The new bile becomes overloaded with cholesterol. This can lead to cholesterol gallstone formation.4
- When you have active Crohn’s disease, you may eat less to limit your Crohn’s disease symptoms. Rapid weight loss is a risk factor for gallstones.2
- Your digestive tract is filled with bacteria. One explanation for the link between Crohn’s disease and gallstones is that certain bacteria become overgrown. These extra bacteria might change bilirubin into a form that can be reabsorbed. The extra bilirubin gets added into bile in the liver. The result is that black gallstones form.4
What are symptoms of gallstones?
Many times, gallstones do not cause any symptoms.3 Symptomatic gallstones may cause steady, moderate-to-severe pain in the upper right part of the abdomen.
What are other risk factors for gallstones?
Besides inflammatory bowel disease disease, other risk factors for gallstones include:2
- Obesity
- Rapid weight loss
- High-calorie, high-refined carbohydrate, low-fiber diet
- Metabolic syndrome or diabetes
How are gallstones evaluated?
If you have symptoms of gallstones, your health care provider will probably need to do an imaging test.3 There are several different ways of looking at your gallbladder. Ultrasound is usually used first because it is inexpensive and effective. A second option is a computed tomography (CT) scan. Your provider will get a better look at the gallbladder and ducts with a CT scan, but this test is more expensive and involves radiation. Magnetic resonance imaging (MRI) may be used as an alternative to a CT scan. Instead of x-rays, an MRI uses magnets and radio waves to take pictures of certain areas of your body.
Other tests that may be used to evaluate gallstones include:
- Hepatobiliary iminodiacetic acid (HIDA) scan. This test involves a (harmless) radioactive chemical and a special camera. Your liver treats the chemical like bile. The technician takes pictures of your liver and gallbladder as the chemical passes through your system.2
- Endoscopic retrograde cholangiopancreatography (ERCP). This procedure combines endoscopy with a contrast material and x-ray. The procedure is done to evaluate problems with the gallbladder and pancreatic ducts. It is sometimes possible to treat gallstones as part of this procedure.7
How are gallstones disease treated?
If the gallstones are not causing symptoms, you may not need treatment.3 Your health care provider may just want to follow-up with you periodically.
When treatment is necessary, the usual treatment is surgery to remove the gallbladder.2 This procedure is called cholecystectomy. Your gallbladder is not an essential organ, so you can live normally without it. The surgery can be done as a minimally invasive (laparoscopic) procedure or an open procedure. Both procedures have the same complication rates. You may be able to go home sooner and recover more quickly after the minimally invasive approach.3
If you cannot have surgery, other treatments include:2,3
- Dissolving the gallstones with medicine (oral dissolution therapy).
- Shock wave therapy to crush the gallstone (shock wave lithotripsy).
What are complications of gallstones?
The complications of gallstones depend on what they are blocking.2 The gallstones can block the cystic duct or common bile duct, which lead away from the gallbladder. This can increase pressure and inflammation of the gallbladder. A gallstone could also block the shared outlet for bile and pancreatic juices. When this happens, the pancreas may become inflamed. Untreated blockages can be fatal.