What Is Crohn’s Disease?
Reviewed by: HU Medical Review Board | Last reviewed: April 2024 | Last updated: May 2024
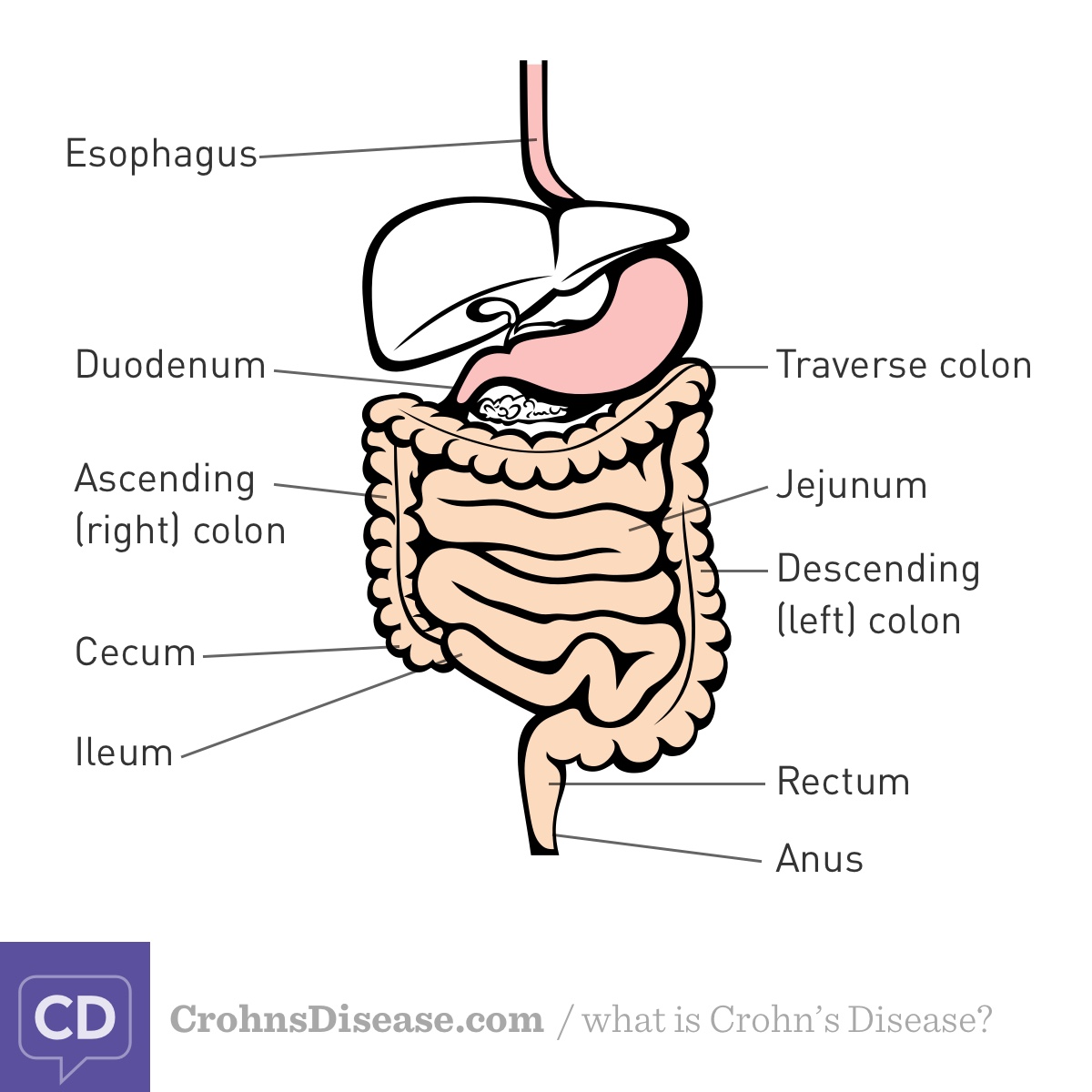
Crohn’s disease is 1 of the 2 main types of inflammatory bowel disease (IBD). Crohn’s is a chronic condition in which inflammation occurs in the gastrointestinal (GI), or digestive, tract. Your GI tract runs from your mouth to your anus, and it is where your body breaks down and absorbs the food you eat.1
In people with Crohn’s, inflammation can occur anywhere along the GI tract. The inflammation is most common at the end of the small intestine (called the ileum) and the large intestine (colon). This inflammation may come and go in a flare-remission cycle. Crohn’s disease typically gets worse over time. You can also have symptoms outside your digestive tract, including in your skin, eyes, and joints.1,2
The other main type of IBD is ulcerative colitis (UC). While UC is similar in some ways to Crohn’s, it affects only the colon. Also, UC affects only the inner lining of the colon, while Crohn’s can affect the entire intestinal wall. Finally, in people with UC, inflammation impacts a continuous section of the colon, always involving at least the rectum though it can extend to the entire colon. In people with Crohn’s, inflammation may "skip," affecting unconnected parts of the GI tract.3
Who is most at risk for Crohn’s disease?
By some estimates, nearly 1 in every 100 people in the United States has Crohn’s disease. Experts are not sure why, but the condition is becoming more common over time. It is more common in urban areas and more developed countries.2-4
Crohn’s affects all genders equally. While Crohn’s is most commonly diagnosed between ages 20 and 30, people may begin to notice symptoms at any age. The condition is diagnosed most often in Caucasian people, but it can affect people of all races and ethnicities.3
People who have certain risk factors may be more likely to develop Crohn’s disease. These risk factors include:1,5
- Having 1 or more family members with Crohn’s disease, especially an immediate family member
- Smoking
- Taking certain medicines, such as some antibiotics, birth control pills, and nonsteroidal anti-inflammatory drugs (NSAIDs)
- Eating a diet high in fat
- Having had appendix removal surgery (appendectomy)
- Living with high levels of stress or depression
What causes Crohn’s disease?
Experts do not know exactly what causes Crohn’s. The condition is likely caused by a combination of several factors, including:1,4,6
- An autoimmune response – This occurs when the body mistakes healthy cells for foreign invaders and begins to attack itself.
- Environmental factors – An overactive immune response may be triggered by things in the environment, such as certain medicines, infections, or toxins.
- Genetics – Researchers have found links between IBD and changes (mutations) in many genes involved in immune function. This is likely why the condition seems to run in families.
The current theory is that Crohn’s disease develops when your immune system overreacts to harmless microorganisms in your digestive tract. Researchers think some people have genes that make them more likely to develop Crohn’s disease. This is called susceptibility. Environmental factors may trigger the overreaction. However, it is not known which environmental factors trigger Crohn’s disease. This is an area of ongoing research.1,4,6
What are the types of Crohn’s disease?
Crohn’s disease is divided into types based on where inflammation occurs along the digestive tract. The main types of Crohn’s are:3,7
- Ileocolitis – Affects the lower part of the small intestine (ileum) and upper part of the colon. This is the most common type of Crohn’s.
- Ileitis – Affects the lower third of the small intestine (ileum).
- Gastroduodenal – Affects the stomach and the top of the small intestine (duodenum).
- Jejunoileitis – Affects the latter two-thirds of the small intestine (jejunum and ileum), causing scattered areas of inflammation.
- Colitis – Affects the lining of the colon.
Figure. Digestive tract
What are the symptoms of Crohn’s disease?
Crohn’s disease can cause a wide range of symptoms, and your specific symptoms may depend on what type of Crohn’s you have. Eating certain foods and experiencing high levels of stress may trigger symptoms or make them worse. The most common symptoms of Crohn’s include:3,6
People living with Crohn’s disease also may experience:6,7
- Extreme tiredness (fatigue)
- Nausea or reduced appetite
- Low red blood cell count (anemia)
- Redness or swelling of the eyes
- Joint pain or soreness
- Fever
- Red bumps under the skin or skin tags
- Sores in the mouth or around the anus
- Kidney stones
- Loss of bone mass (osteoporosis)
What are the possible complications of Crohn’s disease?
Over time, Crohn’s typically gets more severe. It may also become more likely to cause other health problems (complications), including:1,2,7
- Intestinal blockages
- Infected pockets of the digestive tract (abscesses)
- Abnormal tunnels between 2 parts inside the body (fistulas)
- Small tears in the anus (anal fissures)
- Malnutrition from an inability to absorb enough nutrients
- Anemia
- Colon cancer
- Blood clots
How is Crohn’s disease diagnosed?
To diagnose Crohn’s, your doctor will begin by asking you about your personal and family medical histories. They will ask about your symptoms, how long you have had them, and how often they occur.1
Your doctor will also do a physical exam. This exam may include listening to, pressing on, or tapping your abdomen to look for bloating or tenderness.1
Then, your doctor may run several tests to look for further signs of Crohn’s. These tests could include:1,7
- Blood tests – These tests look at your red and white blood cell counts. A high white blood cell count is a sign of inflammation. A low red blood cell count is a sign of anemia.
- Stool tests – With these tests, your doctor can see signs of infection, bacteria, or parasites that may be causing your symptoms.
- Colonoscopy or upper endoscopy – These tests allow your doctor to use a camera inserted into your GI tract to find areas of inflammation.
- Imaging tests – With imaging tests like X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI), your doctor can review pictures of your intestines for damage or inflammation.
How is Crohn’s disease treated?
There is no cure for Crohn’s disease. But treatment can help you manage symptoms, avoid complications, and prevent flares. Common treatments for Crohn’s include:1,8,9
- Medicines – Medicines may decrease inflammation directly or calm the immune system to help lower inflammation. Types of drugs that may be prescribed to treat Crohn’s include aminosalicylates, corticosteroids, immunomodulators, and biologics.
- Bowel rest – To give your bowel a break from processing solid foods, your doctor may suggest that you stop eating for a while. During this time, you will get nutrients from liquids only. The liquids can be given through a drink, a feeding tube, or an intravenous (IV) tube.
- Surgery – More than half of people with Crohn’s will likely need surgery at some point. Surgery may be necessary to treat either severe Crohn’s symptoms or complications that stem from the condition. Surgery may involve removing a part of the intestine or the entire colon.
- Dietary changes – Cutting out or focusing on certain types of foods may help relieve some Crohn’s symptoms. For example, your doctor may suggest avoiding high-fiber foods, fatty foods, and carbonated drinks.
Can Crohn’s be cured?
Currently, there is no cure for Crohn’s disease. People with Crohn’s disease usually have periods of active disease followed by periods of recovery (remission). Studies have shown that, with medical or surgical treatment:7,10
- 50 percent will be in remission or have mild disease for about 5 years
- 45 percent of people in remission will remain relapse-free
- 35 percent of people will have 1 or 2 relapses
- 11 percent of people will continue to have active disease