What is a Fistula?
Reviewed by: HU Medical Review Board | Last Reviewed: January 2018.
A fistula is an abnormal connection between an organ and another structure. Fistulas develop when an organ becomes inflamed or injured. They are a very common complication of inflammatory bowel disease (IBD), occurring more frequently in Crohn’s disease than ulcerative colitis.1 They are especially common when the colon and rectum are involved. About 35% of people with Crohn’s disease have at least 1 fistula.2 Half the time, the fistula has already formed by the time you are diagnosed with Crohn’s disease.2
Where do fistulas occur with IBD?
The most common location for a fistula is around the anus.2 These are called perianal fistulas. Over half of fistulas form in this location. The second most common location is between 2 loops of intestine. Fistulas can also form between the:
- rectum and vagina
- intestine and skin
- intestine and bladder
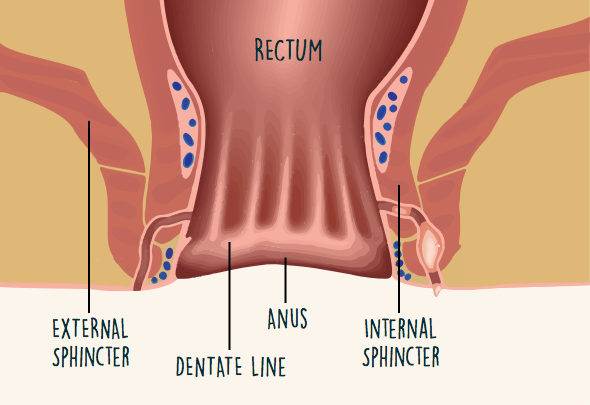
Perianal fistulas are subclassified by their location and complexity (Figure 1).3 You have 2 sphincters, which are muscles that enable you to control bowel movements. These are the internal and external sphincters.
Figure 1. Ano-rectal anatomy
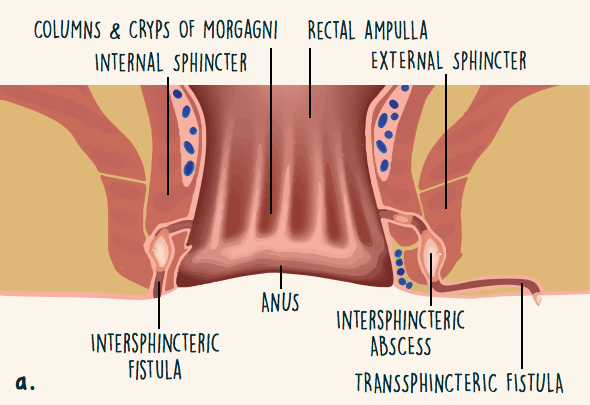
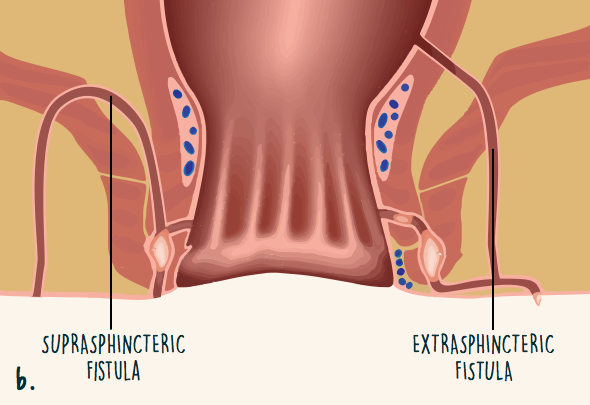
Fistulas can form across 1 or both sphincters (Figure 2).3 They also can form above or between the sphincters. Some fistulas start high up in the rectum and do not cross the sphincters at all. Fistulas can be simple (single tunnel) or complex (multiple tunnels).
Figure 2. Location of perianal fistulas
Symptoms of a fistula with IBD
Symptoms of a fistula depend on where the connection has formed. Fluid or waste may leak continually from the anus or vagina or seep through the wall of the abdomen.2 If you have a perianal fistula, you may have ongoing rectal pain or swelling. A fistula between the intestine and bladder can cause a urinary tract infection that keeps returning. Fistulas between 2 loops of the intestine may not cause any symptoms.4
What are other conditions that can cause a fistula?
Fistulas can form in the digestive tract or perianal region after surgery, radiation therapy for cancer, or traumatic injury.4,5 Some diseases and infections can cause fistulas, such as diverticulitis, sexually transmitted disease, and tuberculosis.
How are perianal fistulas evaluated?
Your health care provider may do a rectal exam when diagnosing inflammatory bowel disease.6 Many people have a perianal fistula at the time they are diagnosed.
After a fistula is identified, the next step is to characterize it. Your health care provider will try to figure out where it connects, how many tunnels there are, and whether you also have an abscess.7
Three main procedures are used to get more information about a perianal fistula:3
- Magnetic resonance imaging (MRI)
- Endoscopic ultrasound
- Rectal examination under anesthesia
Using any two of these three procedures together is a very accurate way of diagnosing perianal fistula.7
MRI (magnetic resonance imaging) uses magnets and radio waves to take pictures of certain areas of your body. MRI reveals the route of the fistula and location of abscesses.3
An alternative to MRI is endoscopic ultrasound. In this procedure, a thin, flexible tube (the endoscope) will be inserted into your rectum. At the end of the tube is an ultrasound wand. This wand uses sound waves to create pictures of the rectum and colon.8
Finally, your health care provider may recommend that you have a rectal examination while you are under anesthesia. During this procedure, your provider will visually examine the fistulas and will attempt to feel where the fistula leads using his/her fingers or probes.9 If necessary, your provider may drain an abscess or place a seton.10 A detailed description of setons is below.
How are they diagnosed?
The procedures used to diagnose internal fistulas include:7
- X-ray with barium contrast material
- MRI
- Computed tomography (CT) scan
How are perianal fistulas treated?
Fistulas can be very complicated to treat. You may need medication and surgery.3,11 Surgery can be risky. Most health care providers will try to treat a perianal fistula with medication first.3 However, many patients with perianal fistulas eventually do need surgery.11
Medications:
Health care providers typically prescribe antibiotics for patients with perianal fistulas. Antibiotics reduce drainage from fistulas.10 Antibiotics are not good for healing fistulas. Therefore, your provider also may prescribe a biologic or immunosuppressant medication.10 Aminosalicylates and corticosteroids do not help perianal fistulas to heal.3,10
Surgery:
Surgical treatment of perianal fistulas can be a multi-step process.11 Surgery is done to drain the fistula and close it permanently.11 A challenge is that many fistulas cross the anal sphincters. The anal sphincters are important for controlling bowel movements. Your surgeon will try to choose a procedure that avoids cutting the sphincters. This reduces the risk of fecal incontinence.7
There are different ways to treat a fistula with surgery (Table).3 These include:
- Helping the fistula heal on its own
- Closing the internal opening with a flap or suture
- Using glue or a plug to close the fistula
- Re-routing digestive waste to avoid the rectum
Table. Surgical Procedures for Treating Perianal Fistula
| Procedure | Description |
|---|---|
| Fistulotomy | The surgeon opens the tunnel surgically, so that it can heal cleanly on its own. For simple fistulas near the skin surface, this procedure is very successful. This procedure is not ideal for fistulas that cross the sphincters. |
| Seton placement | A seton is a thread that looks and feels like a rubber band. The surgeon threads the seton through the fistula. The seton prevents the fistula from closing. By keeping the fistula open, it can drain and the infection can be treated with medication. In some cases, the seton can simply be removed after the fistula has drained and is not inflamed any more. However, many people need a second surgery procedure to close the fistula. This procedure is useful for fistulas that cross the sphincters. |
| Advancement flap | The lining of the rectum is made into a flap that covers the inside opening of the fistula. This procedure works for more than 70% of patients. |
| LIFT (Ligation of the intersphincteric fistula tract) | This procedure is used for fistulas that form between the internal and external sphincters. The inside opening of the fistula is sewn shut. Then the surgeon removes the infected tissue in the tract. This procedure is successful in 58% to 83% of patients. |
| Fibrin glue | For this procedure, the surgeon fills the fistula with a “glue” made of fibrin and thrombin. Fibrin and thrombin are proteins that have a role in clotting. This is a fairly new procedure. The success rates vary widely from study to study.10 |
| Fistula plug | In this procedure, a plug made out of tissue from pigs is implanted in the fistula. The tissue acts like a scaffold. Over time, the patient’s cells fill in the scaffold. Small studies have shown that this procedure is successful in about half of patients. |
| Fecal diversion | If other options have not worked, this procedure is done to re-route digestive waste. The healthy end of the large intestine is attached to a surgical opening in the skin. Digestive waste is eliminated through the small opening called an stoma. This procedure can be temporary or permanent. |
Source: Molendijk I, et al. Best Pract Res Clin Gastroenterol. 2014;28:505-518.
Treating internal fistulas
If an internal fistula is causing symptoms, you may need surgery. If the fistula starts in the large intestine, the surgeon may remove the damaged section. The other end of the fistula is sewn shut.7 This type of surgery is usually done as a minimally invasive procedure (laparoscopically).
Fistulas between the rectum and vagina are also repaired surgically.7 The surgeon repairs these with a flap procedure that is similar to the “advancement flap” technique used to repair perianal fistulas.7
What are the complications?
Studies have shown that at least one-third of people with 1 fistula have another,2 although some estimate are much higher (60%-80%).12
The risks of surgery to repair a perianal fistula can be serious.11 These risks include:
- Losing the ability to control bowel movements (fecal incontinence)
- Narrowing of the anus (anal stenosis)
- Sepsis, a life-threatening reaction to an infection