Dealing with a Partial Bowel Obstruction
Having lived with a form of inflammatory bowel disease (IBD) for almost 17 years now, I have unfortunately dealt with a lot of bowel obstructions and partial obstructions (also known as blockages.) That certainly does not mean that you will have to deal with a lot, or any for that matter, given IBD is hardly a one-size-fits-all disease.
For those of you who do suffer from this because of your Crohn's disease or ulcerative colitis, I wanted to share some of my experiences with you.
My journey with ulcerative colitis
I have lived with a colon (obviously!),a J-pouch, a temporary ileostomy, 5 continent ileostomies, and now a permanent ileostomy.
In addition, I no longer have a rectum or anus. I share this and especially the latter not to be TMI, but to give anyone reading this who is trying to understand more about their own disease and body (or for someone who might be trying to gain more insight for a loved one) some context behind it.
Quite often, I find people share what they have gone through during a particular situation, but leave out some of the back story. For example, if a person is sharing their experiences with how a medication is working for them, wouldn’t it be helpful to know what type of IBD they have? Or what medications they have tried? Or if they have had any surgeries? Do they have an ostomy or a J-pouch? I think you get it.
Featured Forum
View all responsesIt is for this reason that I try to share more of who I am and what my body is like right now so that anyone reading this might be able to tell if what I am saying has anything to do with them or a loved one. I hope that makes sense.
Anyway, I recently suffered from another partial blockage and it got me wanting to share some of my thoughts and some tips I have learned along the way.
What I've learned about bowel obstructions
A bowel obstruction is when your small or large intestine is so blocked that food (or anything else for that matter) is unable to pass through the intestines in a "normal" way. Before I share my personal experiences, I want to clarify that a partial obstruction is very different than a full-on bowel obstruction. For me personally, I can tell the difference in a few ways.
In a partial obstruction, I still have some output while in a true bowel obstruction I would never have an output (AKA stool coming out of a person's stoma or anus) or even bowel sounds.
Both types of obstructions cause my stomach to be incredibly distended and feel discomfort and pain, but with a partial, the pain is more manageable.
The pain from a full blockage
A true blockage is without a doubt one of the most painful things I have ever experienced
 It seems to be constant pain with waves of it getting much, much more severe. Kind of like labor contractions in a way. It also causes a lot of nausea and vomiting.
It seems to be constant pain with waves of it getting much, much more severe. Kind of like labor contractions in a way. It also causes a lot of nausea and vomiting.
With a partial obstruction, I don't have this block – so to speak – in my mind telling me not to eat. When I am in the midst of a full blockage/obstruction, I cannot even think about consuming any food or liquids. If I do in an attempt to flush things out of my system, it will almost always make things worse or cause me to vomit.
A bowel obstruction can be an emergency
If you are experiencing a true bowel obstruction, please call your GI or surgeon and get yourself to a hospital ASAP. I don't say things like that lightly because I know how awful it is to have to go to the ER or be inpatient in the hospital. Like a lot of you reading this, I look at it as the absolute last resort. However, an obstruction can be very dangerous and cause a lot of complications the longer you wait to seek medical attention. Not to mention, your pain will become increasingly worse and the frequency at which your body is throwing up will increase.
If you are not in severe pain (trust me, you will know the pain I am referring to if it happens to you) and have some stool output either through your stoma or rectum/anus, it is most likely a partial obstruction. That does not mean you should just go about your day and forget what is happening to your body. It means you have been given a chance to help yourself before it gets to a more dire state. I would also never deter anyone from calling their doctor or going to a local emergency room if they are scared of what is going on and want to err on the side of caution. You can never be too careful when it comes to a disease as complex as IBD.
**If your partial obstruction ends up turning into a full-blown blockage, that does NOT mean it is YOUR fault!**
Common causes in Crohn's and ulcerative colitis patients"
- Undigested food
- Strictures, which are narrowing of the intestines
- Prior abdominal surgery since adhesions could be present; therefore, the more surgeries a person has, the more adhesions there probably are in the abdomen
Helpful things when suffering from a blockage
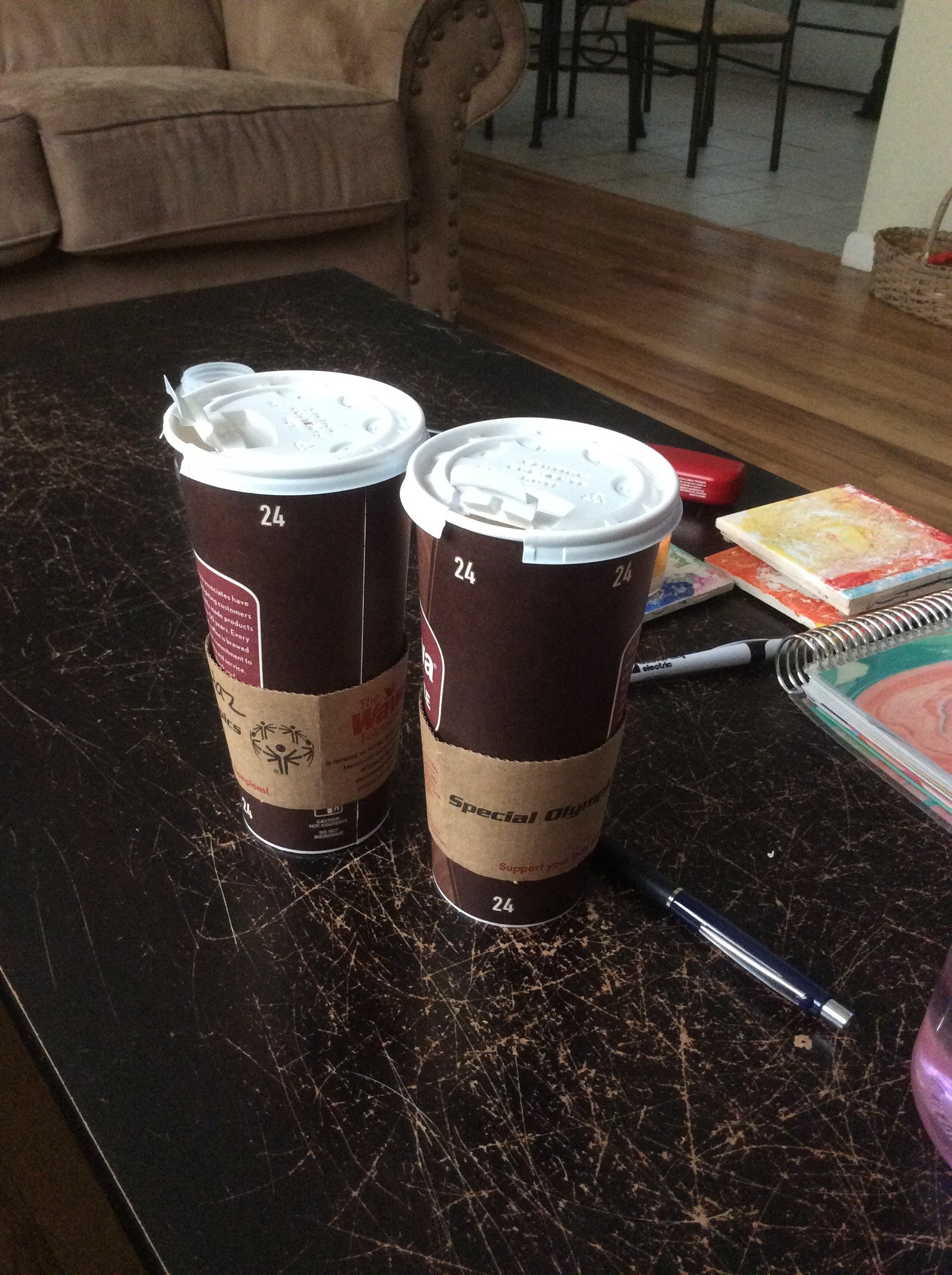
- Hot coffee (I always go with decaf but I am sure regular coffee would have the same result)
- Hot tea
- Milk (Many people who suffer from IBD cannot tolerate lactose or dairy well. While usually this means someone probably wants to stay away from foods that contain this, it also might have a laxative effect on the body which could aid in flushing your system out. In fact, any beverage that has this impact on your intestines could help unless it causes you a great deal of pain and suffering in another way.
I find heating pads to be soothing to lay on your stomach.) - Moving your body a little has also been known to help get things flowing again.
A bowel obstruction with UC or Crohn's can be scary
To any of you reading this who suffer from frequent bowel obstructions of any kind, please know you are so far from alone. It is fairly common in those who have severe Crohn's disease or ulcerative colitis. I know how scary they are and how unpredictable they can be. I always try to pinpoint it to food since it is how I try to control a lot of my symptoms. While sometimes it is food-related (which makes me happy since I know I just need to avoid whatever that triggering food was and I will be okay), other times I cannot. Enter frustration overload.
Do you experience bowel obstructions frequently? Are they usually partial or worse? Do you usually have to go to the ER/hospital? Have any tips for others?

Join the conversation