Living with UC and Pouchitis
I lived with UC and pouchitis for many years – the majority of the time I had my J-pouch, actually.
I was diagnosed with ulcerative colitis in 2007, but my colon was whipped out before I even had time to really process what that even meant. Because I'd been so unwell, the recovery was a long one. One year after that, I had surgery to create my J-pouch. A J-pouch is basically a replacement rectum, built from loops of small intestine and connected to the anus.
I experienced pouchitis quickly
My first experience of pouchitis was before I was even using my J-pouch! It wasn't even connected yet, and I started experiencing tenesmus (that cramping in the rectum feeling) and urgency, due to inflammation. Of course, the urgency was only to pass the mucous my intestine was creating.
I had a course of steroids and used foam enemas at night to calm the inflammation down. I should have known then that it wasn’t going to be an easy ride.
Looking for more info about ulcerative colitis
A year after it had been created, I had the J-pouch connected up. I expected the recovery from having it connected to be difficult, based on the booklet I'd been given from the hospital and what I'd read online. It was 2009, so I had not been talking to other people in the IBD community yet. I literally just looked it up online on a library PC. The information wasn't very patient-orientated.
I thought I was going to have to retrain my muscles, but that wasn't the case for me. I think, both fortunately and unfortunately, the fact that I'd had pouchitis in my pouch before it was even connected had meant that my muscles had still had to work to "hold it in."
I was glad to be free of my stoma
I was thrilled to be free from my ileostomy. I'd had a really difficult time with it due to leaks and burnt skin. I now realise that I should have received better support and care from my healthcare team, but I didn't know that then. I thought that's what life with a stoma always was, so it had impacted my mental health a lot.
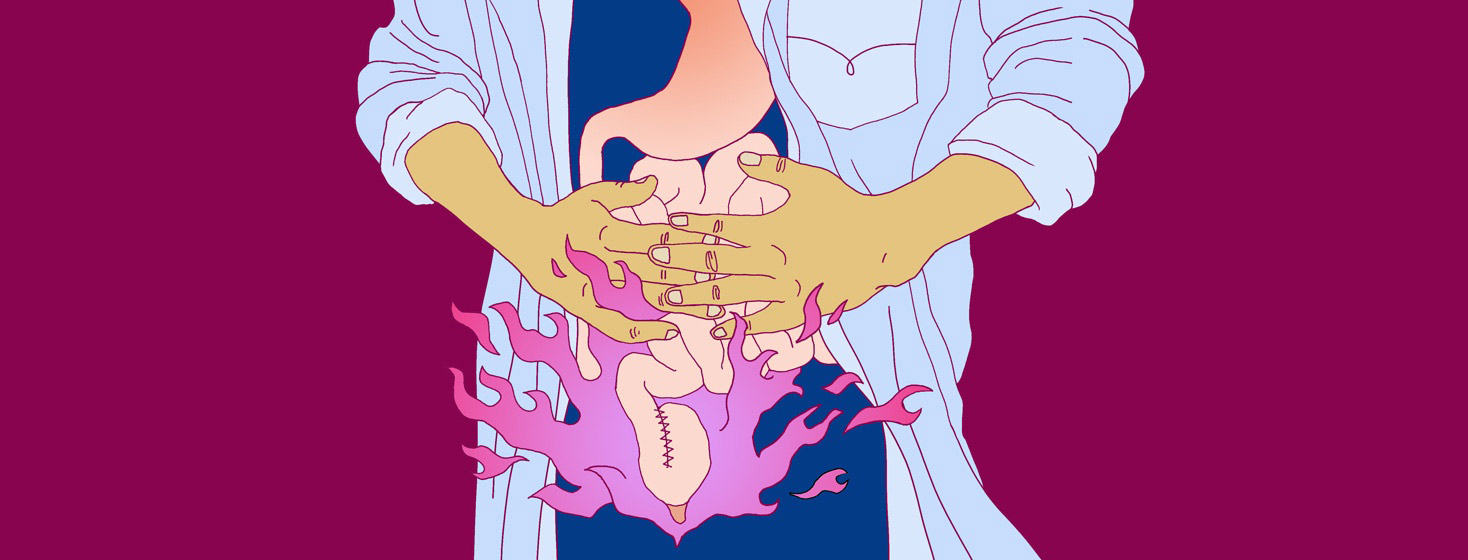
Pouchitis was a constant battle
It didn’t take long for pouchitis to raise its ugly head again. I had constant abdominal cramps, and it was tender to touch. Toilet trips were frequent and urgent, and the tenesmus was back. Sometimes, it was so inflamed I could feel my pouch move with every footstep I took.
Between having it connected in 2009 and 2014, I'd had constant scopes to confirm that I had active pouchitis. The antibiotics that are usually prescribed for it here in the UK didn't help ease my symptoms.
Featured Forum
View all responsesA brief UC remission
I tried combinations of antibiotics and prescription probiotics, but the only thing that was helping me was steroids (prednisone). Eventually, I couldn't wean off the steroids because the flare returned when I started tapering (lowering) my dose. I then moved on to azathioprine, and I had a wonderful 10-month remission! It was blissful.
Finally, I could go to festivals and out with friends without the constant need for painkillers and a toilet map! But I began flaring again in 2014, during a particularly stressful period involving a bad break-up and a swift house move. Money was tight and that was difficult, too.
Ongoing pouch problems
The plan was to start infliximab. In preparation, I had a chest X-ray, blood tests, and a flexible sigmoidoscopy. That scope led to the identification of some severe strictures (narrowed areas of intestine), that they couldn't get the scope through. More tests were ordered to get a better look.
My IBD nurse said I needed to start thinking about the possibility of a pouch excision and wanted me to see the colorectal surgeon. I asked to be referred to another hospital, as I'd had traumatic experiences there.
Surgery and an unplanned pouch rest
Those additional tests led to an emergency surgery to remove an abscess and to untwist my intestine, thankfully at the new hospital. I woke up with an ileostomy again because my pouch had been ripped during the surgery, and it needed time to heal.
I was already heavily involved in the online IBD community by then, so I'd learnt a lot about ostomies. That, and the fact that the new stoma was simply built better, meant my experience with it was completely different to my first one. I was able to enjoy life again, and apart from the loperamide to thicken up my output, I was medication- and pain-free!
I debated not having the J-pouch re-connected, but the surgeon said it might behave better after its rest. So I thought I'd give it a go so I didn't always wonder "what if?"
Pouchitis after the pouch rest
It didn't behave better. Shortly after being reconnected, pouchitis came again. Oddly, the symptoms differed. I experienced a lot of trapped wind, which had never happened before. This time, there was blood in my stool, too.
Scopes confirmed bleeding ulcers in my J-pouch, which I'd not had when my J-pouch had been connected previously. Flares had always involved inflammation, but never ulcers.
Continued complications
My IBD team said we had to think about it like a new pouch, due to its rest, so we had to start from square 1 with treatment options rather than just heading straight to infliximab. I didn't have prednisone again. My IBD team felt I’d had my quota for life. I didn't want it anyway because it had affected my mental health so badly the time before.
I tried all of the other medications I'd tried previously plus infliximab. It became clear that the best thing for my quality of life was to remove the pouch in favour of a permanent ileostomy.
J-pouch excision
I asked to be referred back to the surgeon and hospital I'd had my previous 2 surgeries at. My IBD team was very accommodating, and I eventually had my J-pouch removed in 2018.
Sometimes, I can't help but regret my decision to have the J-pouch, but there really is no point in looking back and wondering "what if." I can't change anything now. It's just a shame so many years of my life passed me by, whilst I felt like all I could do was exist rather than actually live it.
Ulcerative colitis certainly is a journey
I'm in a better place now, physically and mentally, despite having secondary fibromyalgia and bladder muscle dysfunction following my last surgery. In some respects, I feel very lucky. I have some wonderful friends, who I only met because of my journey and online activity in the IBD community. I love my job, and that's something that would never have happened if my life hadn't gone the way it has.
Funny, things always seem to work out in the end.
Join the conversation